Bone injuries in the face and skull—known as craniomaxillofacial defects—can be caused by sports injuries, vehicle accidents, or battlefield injuries. Repairing such defects is complicated because different types of cells need to interact with each other. In a new study, researchers are investigating the types of material used in reconstruction to see which one works best.
“Our lab focuses on developing degradable biomaterials – also known as scaffolds – for bone and tissue repair,” said Vasiliki Kolliopoulos, a graduate student in the Harley lab. “There are many types of cells in the bone environment that contribute to healing, including stem cells that form bone, and monocytes that help with the immune response. This study investigated how the scaffold material affects the combined behavior of these different cells.”
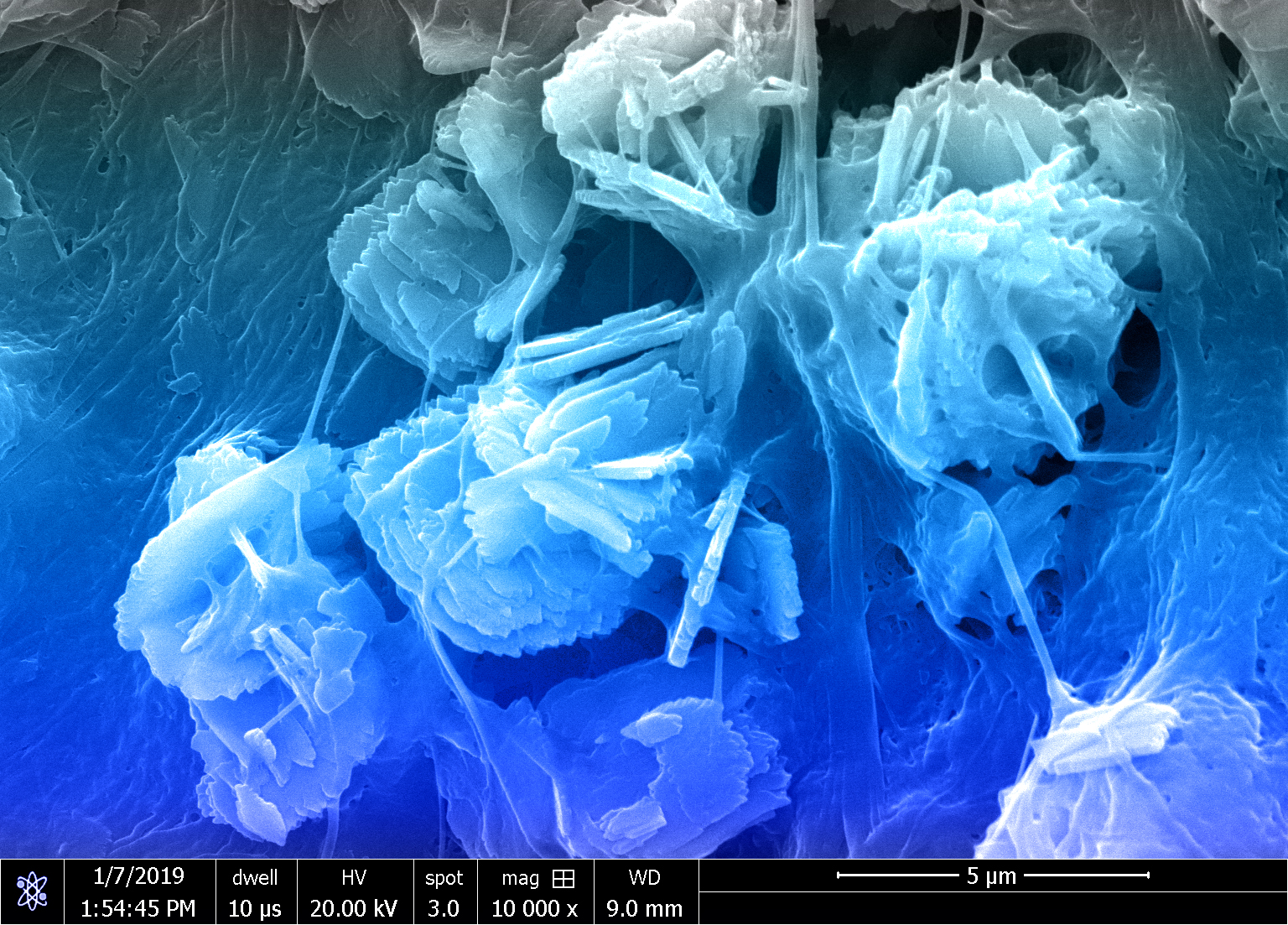
The researchers adapted a collagen biomaterial to include one of three different types of GAGs found in the bone tissue microenvironment: chondroitin-4-sulfate, chondroitin-6-sulfate, and heparin. They then investigated how these GAGs influence processes important to bone regeneration such as stem cell activity, immune cell activation, and endothelial cell activity, which is important for the formation of new blood vessels.
To do so, stem cells were added to the scaffolds and the surrounding solution, or media, was collected for up to twenty-one days. Stem cells are powerful factories of molecules that may influence other cells in the wound environment. After being collected, the conditioned media was added to cultures of endothelial cells, which are found in blood vessels. “Bone regeneration requires the growth of blood vessels and not many people have looked at how scaffold materials affect endothelial cells and how it could improve bone repair,” said Marley Dewey, a former graduate student in the Harley lab.
The researchers tracked the growth of the endothelial cells for 6-12 hours. “Although heparin is known to directly influence blood vessel formation, to our surprise we saw that the media generated by stem cells in chondroitin-6-sulfate scaffolds led to the greatest amount of blood vessel development compared to the other two scaffolds,” Kolliopoulos said.
The conditioned media was also studied to determine the types of molecules, known as soluble factors, that aid in blood vessel and bone development. Finally, the researchers added the conditioned media to monocytes and tracked their growth for 21 days to measure the types of immune cells they turned into. They found that the types and number of soluble factors were different for each scaffold type, and chondroitin-6-sulfate media produced the greatest number of immune cells that help during an inflammatory response.
The researchers are planning to further investigate the responses of the immune cells. “Stem cells can signal to monocytes when your body sounds the alarm that something is wrong. Therefore, we want to see whether the stem cells that are grown in the scaffolds in an inflammatory environment will secrete a different cocktail of soluble factors,” Kolliopoulos said.
“These results show that the soluble factors play an important role in these multicellular systems,” Kolliopoulos said. “We showed that there are differences in the cell responses depending on what material is used and it is important to understand these interactions before you move on to more complicated experiments.”
It is unclear what aspect of the scaffold material is contributing to the differences in growth factors and cell growth, a problem the Harley lab plans to tackle next. “After we identify how the scaffolds influence the cells, we want to combine the different cell types to see what happens,” Kolliopoulos said. “We are trying to develop biomaterials that will be used by surgeons to repair bone defects. Understanding what these materials do to multiple cell types is important.”
Mai Ngo, the third author on the paper, helped in understanding the blood vessel development. The paper “Glycosaminoglycan content of a mineralized collagen scaffold promotes mesenchymal stem cell secretion of factors to modulate angiogenesis and monocyte differentiation” was published in Materialia and can be found at https://doi.org/10.1016/j.mtla.2021.101149.
The work was supported by the National Institute of Dental and Craniofacial Research of the National Institutes of Health, the NSF Graduate Research Fellowship, and the Chemistry-Biology Interface Research Training Program at the University of Illinois.